Trabeculectomy and Express Mini-Shunt Procedures
If you have glaucoma and medications and laser surgeries do not lower your eye pressure adequately, your eye doctor may recommend a procedure called a trabeculectomy. This procedure is often performed with use of an anti-scarring medication to reduce the risk of scarring. There is also an option to implant an ExPress mini-shunt under the flap which may reduce the short term complications of the surgery.
During this procedure which is performed in an operating room on an outpatient basis, a tiny drainage opening is made underneath a flap or trap-door of the sclera (white of the eye). The new opening allows fluid from inside the eye to flow underneath the edges of the flap to raise a filtration site within the conjunctiva (outer layer of the eye) called a “bleb”. The bleb is mostly hidden under the eyelid and is often quite low and spread over a large area. The aqueous humor diverted to the bleb then gets re-absorbed by surrounding blood vessels. When successful, the procedure will lower your intraocular pressure (IOP), minimizing the risk of vision loss from glaucoma.
Some of the risks and complications from trabeculectomy surgery include the following:
- infection;
- bleeding in the eye;
- swelling in the eye;
- cataract (in cases where cataract has not already been removed); and
- decreased or lost vision;
- failure to control intraocular pressure, with the need for another operation
- eye pressure that is too low;
- irritation or discomfort in the eye.
Aqueous Shunt Surgery
Aqueous Shunt Surgery is used as an alternative to trabeculectomy or Express mini-shunt when there is a high likelihood that those procedures would be ineffective or fail. Patients with neovascular glaucoma, uveitic glaucoma, or scarring from previous ocular surgeries are good candidates for aqueous shunt surgeries. There are several types of aqueous shunts available. Dr Ochsner is experienced at implanting all of them and will select the one most likely to provide adequate control of your glaucoma.
These procedures are also performed as an outpatient and carry similar risks as trabeculectomy.
Cylclophotocoagulation
When attempts to lower eye pressure by bypassing the blockage to aqueous outflow fail, another treatment option is to reduce the amount of aqueous entering the eye. Cyclophotocoagulation is a procedure that uses a laser to treat the part of your eye that produces the aqueous, the ciliary body. This procedure does not require an incision but is done in the outpatient operating room while you are sedated.
Glaucoma Laser Treatments
Laser surgeries have become important in the treatment of different eye problems and diseases. There are several types of laser surgery used to treat glaucoma.
The type of laser surgery will depend on the form of glaucoma and how severe it is. Lasers produce a focused beam of light that can make a very small burn or opening in your eye tissue, depending on the strength of the light beam. Laser surgeries are performed in an outpatient setting in your doctor’s office or in a hospital clinic.
During the laser surgery, the eye is numbed so that there is little or no pain. The eye doctor then holds a special lens to the eye. The laser beam is aimed into the eye, and there is a bright light, like a camera flash.
Laser Treatments for Open Angle Glaucoma
Selective Laser Trabeculoplasty (SLT)
For the treatment of primary open-angle glaucoma (POAG).
SLT uses a laser that works at very low levels. It treats specific cells “selectively,” leaving untreated portions of the trabecular meshwork intact. For this reason, SLT may be safely repeated.
SLT may be an alternative for those who have been treated unsuccessfully with ALT or pressure-lowering drops. SLT has successfully lowered eye pressure in up to 75% of patients treated.
Argon Laser Trabeculoplasty (ALT):
For the treatment of primary open-angle glaucoma (POAG).
The laser beam opens the fluid channels of the eye, helping the drainage system work better. In many cases, medication will still be needed.
Usually, half the fluid channels are treated first. If necessary, the other fluid channels can be treated in a separate session another time. This method prevents over-correction and lowers the risk of increased pressure following surgery.
Laser Treatment for Narrow or Closed Angle Glaucoma
Laser Peripheral Iridotomy (LPI)
For the treatment of narrow angles and narrow-angle glaucoma.
Narrow-angle glaucoma (also known as angle-closure glaucoma) occurs when the angle between the iris and the cornea in the eye is too small. This causes the iris to block fluid drainage, increasing inner eye pressure. LPI makes a small hole in the iris, allowing it to fall back from the fluid channel and helping the fluid drain.
Laser Treatments for Other Glaucomas
Laser Cyclophotocoagulation
An alternative to filtering microsurgery that is typically used later in the treatment algorithm. Several different types of lasers can be used to hamper the ciliary body’s ability to make fluid and, thus, lower the eye pressure. The procedure may need to be repeated in order to permanently control glaucoma.
What to Expect During and After Glaucoma Laser Treatment
Pain or Discomfort from Glaucoma Laser Surgery
There is a slight stinging sensation associated with LPI and ALT. In YAG CP laser surgery, a local anesthetic is used to numb the eye. Once the eye has been numbed, there should be little or no pain and discomfort.
Long-term Benefits of Glaucoma Laser Surgery
Glaucoma laser surgeries help to lower the intraocular pressure (IOP) in the eye. The length of time the IOP remains lower depends on the type of laser surgery, the type of glaucoma, age, race, and many other factors. Some people may need the surgery repeated to better control the pressure IOP.
Medication Following Laser Surgery
In most cases, medications are still necessary to control and maintain eye pressure. However, surgery may lessen the amount of medication needed.
Recovery Time
In general, patients can resume normal daily activities the next day after laser surgery.
The procedure is usually performed in an eye doctor’s office or eye clinic. Before the surgery, your eye will be numbed with medicine. Your eye may be a bit irritated and your vision slightly blurry after the surgery. You should arrange a ride home after your surgery.
Risks of Laser Surgery
As with any type of surgery, laser surgery can carry some risks. Some people experience a short-term increase in their intraocular pressure (IOP) soon after surgery. In others who require CyclophotoCoagulation, there is a risk of the IOP dropping too low to maintain the eye’s normal metabolism and shape. The use of anti-glaucoma medication before and after surgery can help to reduce this risk.
Increased Risk of Cataracts
There is a small risk of developing cataracts after some types of laser surgery for glaucoma. However, the potential benefits of the surgery usually outweigh any risks.
It is important to discuss all of your questions or concerns about laser surgery with Dr. Ochsner.
Minimally Invasive Glaucoma Surgery
For More information visit http://migs.org/
TRAB 360 – Transluminal Trabeculotomy Technique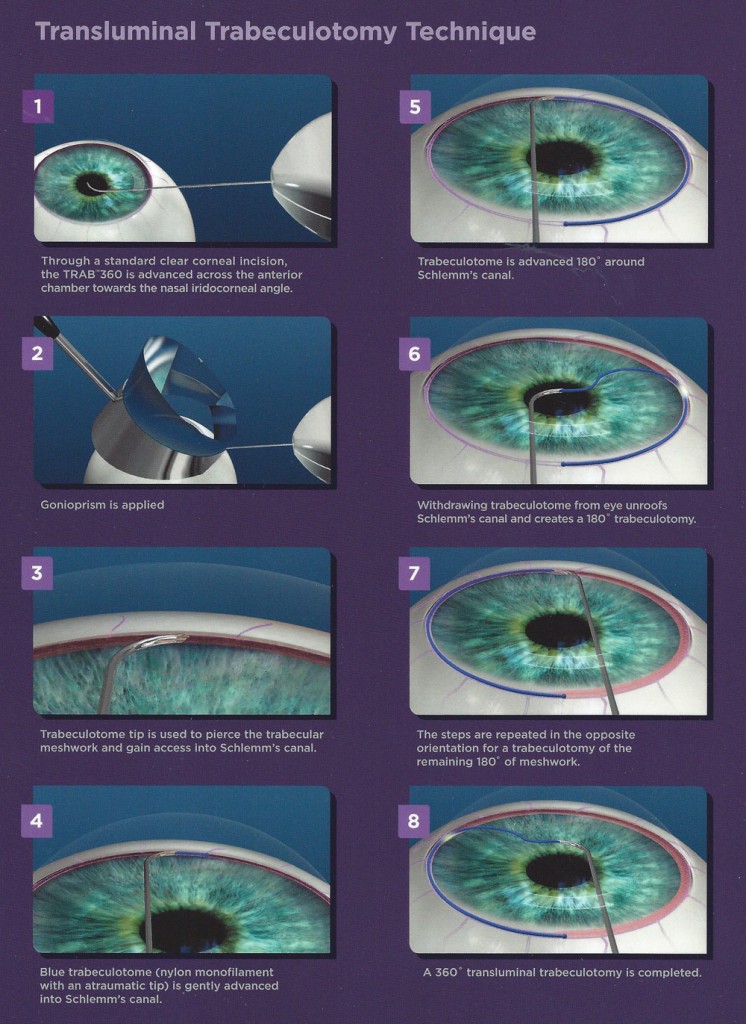
VISC 360 – Viscodilation Technique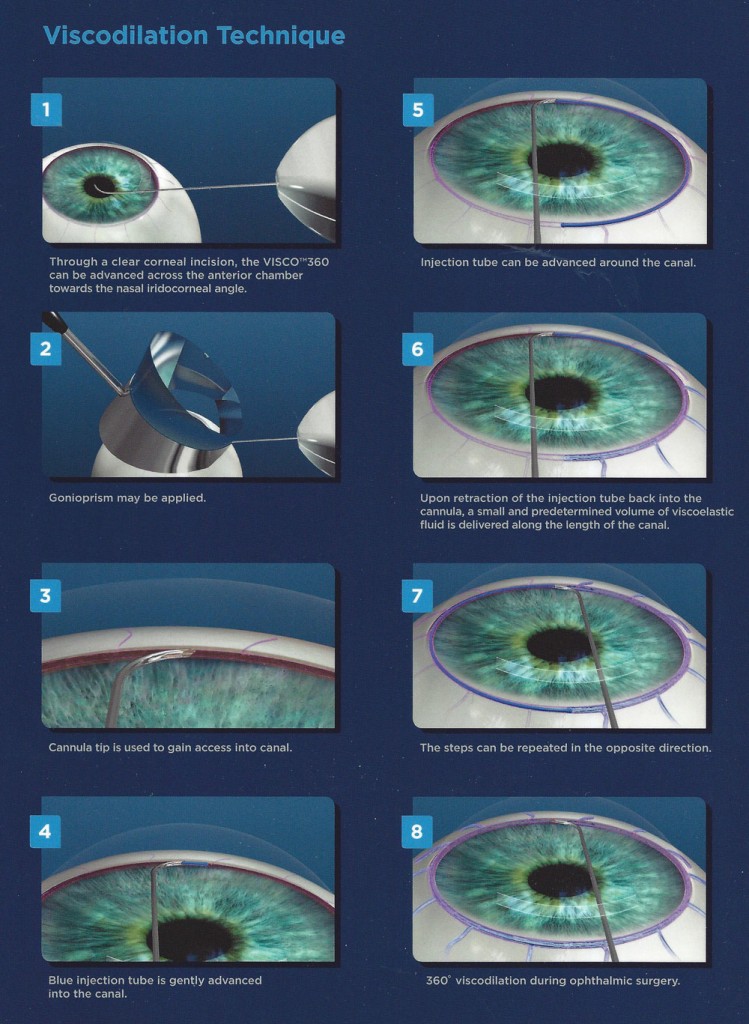
iStent – the world’s smallest medical implant delivers big results in mild-to-moderate open-angle glaucoma.
For More information visit http://migs.org/istent
While mild-to-moderate open-angle glaucoma is very common, many people are unaware of their condition, especially in the early stages, when their vision may be unaffected. In many people, open-angle glaucoma is characterized by an increase in the intraocular pressure (IOP) of your eye. This pressure is caused by the buildup of fluid within the eye. Too much fluid raises pressure, which can cause the gradual loss of vision. And while glaucoma moves slowly, its damage is irreparable.
The world’s tiniest medical device—iStent—is 20,000 times smaller than the intraocular lenses (IOL) used in your cataract surgery. But the size of iStent is only part of its story. By increasing the eye’s ability to drain fluid, this technology is designed to reduce the pressure in your eye.
How does iStent work?
iStent works like the stents used to prevent heart attacks and strokes. When blood vessels get clogged, a stent creates access to the vessel flow. While a highly innovative technology, how iStent works is elegantly simple:
- If you have glaucoma, over time the eye’s natural drainage system becomes clogged
- iStent creates a permanent opening through the blockage to improve the eye’s natural outflow
- Restoring this mechanism lowers and controls pressure within the eye
Trabectome
For More information visit http://migs.org/
The Trabectome, an FDA-cleared device for minimally invasive surgical treatment of open-angle glaucoma, is designed to improve fluid drainage from the eye and balance intraocular pressure (IOP).Trabectome can help to stabilize optic nerve health and minimize further visual field damage by gently unblocking pressure with a three-step process that takes approximately 30 minutes. You will go home the same day!
- Incision– a tiny incision is made across the chamber of the affected eye.
- Electro-surgical pulse- diseased tissue is removed with an electrosurgical pulse.
- Washout– the eye is washed out with saline to remove tissue debris.
What are the Advantages of Trabectome surgery?
- Minimally Invasive
- Restores the eye’s natural fluid balance
- Low patient risk
- Simpler than traditional therapies
- Low complication rate
- Easily combines with cataract extraction
- Safe, economical and effective
XEN Gel Implant
The XEN Gel Implant is a very small flexible tube that creates a new pathway for fluid to drain from the eye, reducing eye pressure. For more information visit http://migs.org/xen/
CyPass Micro-Stent
The CyPass Micro-Stent is a very small tube that is implanted just below the surface of the eye, lowering eye pressure and reducing or eliminating the need for glaucoma medications. For more information visit http://migs.org/cypass/
Endoscopic Cyclophotocoagulation (ECP)
A laser procedure performed at the same time or after cataract surgery to lower eye pressure. For more information visit http://migs.org/endoscopic-cyclophotocoagulation/
MicroPulse Cyclophotocoagulation (MPCPC)
A non-invasive laser treatment of the part of the eye that produces fluid. Designed to allow tissue to cool between pulses, minimising tissue damage. For more information visit http://migs.org/micropulse-cyclophotocoagulation/


 Located at Howe Creek Landing
700 Military Cutoff Rd., Suite 202
Wilmington, NC 28405
Located at Howe Creek Landing
700 Military Cutoff Rd., Suite 202
Wilmington, NC 28405